Airway Assessment
Assessment of a patient's airway, and your likely ability to safely secure an adequate airway is critical prior to to anaesthesia. The outcome of your assessment should inform your airway plan.
History
Taking an airway history is critical to planning airway management. This should include:
-
Does the patient have a known difficult airway?
-
Do they have a letter? If so, examine this
-
What was the previous difficulty? Difficulty with bag-valve-mask ventilation is different to difficulty with LMA insertion, which is different in turn to intubation
-
What was the seniority of the operator? A junior trainee reporting a difficulty airway may not carry the same weight as a senior specialist
-
When was the difficult airway reported? Training and technology (eg video laryngoscopy) have advanced markedly in recent decades
-
What technique was successfully (if successful!) used
-
-
What surgery is the patient undergoing? Surgery or pathology involving the head, neck, or chest may cause airway challenges
-
Does the patient have any risk factors for a difficult airway, for example reduced neck range of movement (eg in rheumatoid arthritis)
-
Does the patient have any known airway obstruction which could affect anaesthesia, eg obstructve sleep apnoea?
-
Is any relevant imaging available? If so, examine this along with any available specialist reports
-
Are any relevant specialist letters available, eg letters from ENT clinics?
-
Are previous anaesthetic charts available? These must be scrutinised, specifically around the airway management technique
Examination
-
Cardiovascular and Respiratory examination should be performed on all patients prior to anaesthesia
There are multiple methods by which airway assessment can be performed. None, unfortunately, are 100% sensitive and specific. All have their advantages and disadvantages. Some of the more common are listed here:
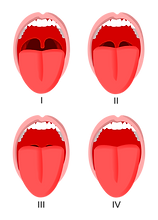
Mallampati (image sourced from https://commons.wikimedia.org/wiki/File:Mallampati.svg#Licensing):
-
Soft palate can be completely visualised
-
Uvula can be completely visualised
-
Only base of uvula can be visualised
-
Soft palate is not visible
Some mnemonics aid airway assessment:
LEMON assessment (for ease of intubation)
-
L ook externally for indicators of difficult airway, eg stature, small mouth, beard. If present, greater intubation difficulty predicted
-
E valuate 3-3-2 rule (can the patient fit 3 fingers between their incisors, is the distance from the mentum to hyoid >3 finger widths, is the thyro-hyoid distance >2 finger widths. If not, greater intubation difficulty is predicted
-
M allampati score (3 or 4 predict greater intubation difficulty)
-
O bstruction/obesity predict greater intubation difficulty
-
N eck extension is critical for direct laryngoscopy. Inability to extend the neck for any reason (eg C spine collar, rheumatoid arthritis) predicts intubation difficulty
RODS assessment (for ease of LMA insertion)
-
R educed mouth opening
-
O bstruction
-
D istorted airway
-
S tiff lungs
BONES assessment (for ease of bag-valve-mask ventilation)
-
B eard
-
O besity
-
N o teeth
-
E lderley
-
S leep apnoea/snores